March update
It's been a full month! Archives are always available on the website. Thanks for sharing with colleagues who might find these summaries useful.
Hey everyone,
If you read nothing else this March, be sure to enjoy DeLancey’s expert review of pelvic floor injuries following childbirth. He has devoted his life to pelvic floor biomechanics and urogynaecology, and it’s just wonderful.
Other highlights include:
A Swedish nationwide cohort study investigating the neurodevelopmental outcomes of children born moderately or late preterm
A case report detailing the successful use of extracorporeal CPR and percutaneous catheter-based interventions in managing peripartum PE.
A NEJM randomised trial comparing simple and radical hysterectomy for low-risk cervical cancer.
Brain morphology in children aged 7-15 years after in utero SSRI exposure.
Final additions: FDCS and the risk of PTB (don’t we love our acronyms), Kypros on aspirin to prevent PTB and the challenge of distinguishing necessary vs unnecessary discomfort during specialist training in O&G.
These summaries highlight the breadth of ongoing research and advancements in various areas of medicine, from obstetrics and gynaecology to neonatology and critical care. All from the last few weeks!
Cheers for now,
Danny
Pelvic floor injury during vaginal birth is life-altering and preventable: what can we do about it?
DeLancey, John O.L. et al. “Pelvic Floor Injury during Vaginal Birth Is Life-Altering and Preventable: What Can We Do about It?” American Journal of Obstetrics and Gynecology 230, no. 3 (March 2024): 279-294.e2.
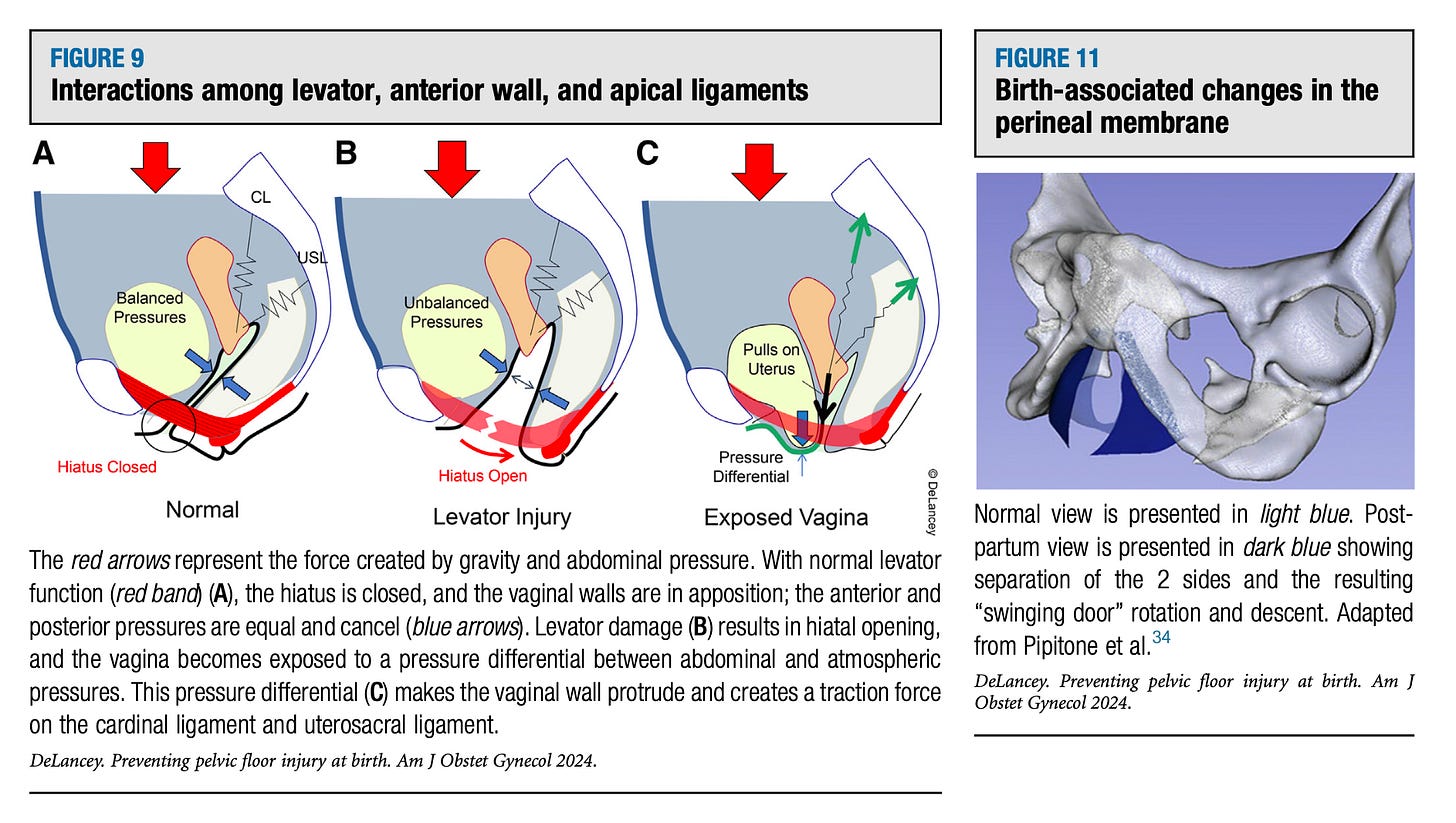
Pelvic floor disorders, such as prolapse and stress incontinence, are distressing and common consequences of childbirth that can have lifelong impacts on women's health and quality of life. This expert review by DeLancey et al. provides a comprehensive overview of the current understanding of pelvic floor injuries during vaginal delivery, their long-term sequelae, and potential strategies for prevention and management.
The authors highlight the critical role of levator ani muscle and tissue overstretching in the development of these disorders, with up to 19% of primiparous women experiencing visible muscle tears on imaging.
They also discuss the multifactorial risk factors for levator injury, including forceps delivery, occiput posterior birth, and high birthweight, as well as possible preventive measures such as manual rotation, gradual delivery, and early labour induction. The review emphasises the importance of early recognition, physical therapy, and patient education in providing care for affected women and empowering them to make informed decisions about their labour management.
Maternal Depression, Prenatal SSRI Exposure, and Brain Trajectories in Childhood
Koc, Dogukan et al. “Prenatal Antidepressant Exposure and Offspring Brain Morphologic Trajectory.” JAMA Psychiatry 80, no. 12 (December 1, 2023): 1208. https://doi.org/10.1001/jamapsychiatry.2023.3161.
Maternal depression during pregnancy is a common condition, often treated with selective serotonin reuptake inhibitors (SSRIs). While these medications are generally considered safe, preclinical studies suggest that gestational SSRI exposure may adversely affect offspring brain and behavioural development. However, untreated maternal depression also poses risks to the fetus, creating a challenge for healthcare providers.
Studies in children and adolescents have reported mixed findings, with some suggesting increased rates of neurodevelopmental disorders and mental health issues, while others attribute these outcomes to the mother's underlying illness or shared genetic and environmental factors.
Koc et al. conducted a longitudinal study using data from the Generation R cohort to examine the association between maternal SSRI use during pregnancy and altered brain development in offspring from childhood (age 7) to midadolescence (age 15).
The study found that children exposed to SSRIs in utero had lower grey matter volume, including in corticolimbic regions, which persisted into adolescence. Reduced white matter and amygdala volumes were observed at age 7 but normalised over time. Article and Editorial here.
Simple versus Radical Hysterectomy in Women with Low-Risk Cervical Cancer
Plante, Marie, et al. “Simple versus Radical Hysterectomy in Women with Low-Risk Cervical Cancer.” New England Journal of Medicine 390, no. 9 (February 29, 2024): 819–29.
Last month’s NEJM published a multicentre, randomised, non-inferiority trial comparing radical hysterectomy with simple hysterectomy plus lymph node assessment in 700 patients with low-risk cervical cancer.
The primary outcome, pelvic recurrence at 3 years, occurred in 2.17% of patients who underwent radical hysterectomy and 2.52% who underwent simple hysterectomy, demonstrating similar outcomes. The simple hysterectomy group had lower risks of urinary tract complications and better quality of life and sexual function measures.
While these findings challenge current standards, accurate patient selection based on tumour size and depth of invasion is critical. The study's limitations include the lack of central pathological or radiologic assessment, and the generalisability to patients with high-grade tumours or lymphovascular invasion remains unclear.
Also this study doesn’t address the question of surgical approach. Results from the Laparoscopic Approach to Cervical Cancer (LACC) trial showed that minimally invasive radical hysterectomy was associated with lower rates of disease-free survival and overall survival than the open approach in patients with early stage cancer. Full article and NEJM Editorial below.
Transition to Adulthood for Extremely Preterm Survivors
Pigdon, Lauren et al. “Transition to Adulthood for Extremely Preterm Survivors.” Pediatrics 153, no. 1 (January 1, 2024): e2022060119
How is that 26 weeker you delivered by classical CS doing? How is she going to do when she’s an adult? Survivors born extremely preterm (EP; <28 weeks) or with extremely low birth weight (ELBW; <1000 g) face increased risks of neurodevelopmental impairments and functional challenges compared to term-born peers.
However, most studies have focused on cohorts born before the introduction of exogenous surfactant in the early 1990s, which dramatically improved survival rates. It remains unclear how EP/ELBW individuals born in the ‘surfactant era’ fare during the critical transition to adulthood.
Pigdon et al. compared the transition to adulthood of EP/ELBW survivors born in 1991-1992 to term-born controls. The study found that EP/ELBW adults had similar rates of high school completion, employment, and romantic relationships.
However, they were more likely to have government income support, live with parents, and have lower engagement in risk behaviors like smoking and substance use. Some evidence suggested fewer EP/ELBW individuals attended university. The findings indicate that while EP/ELBW survivors are transitioning well in many areas, challenges remain in independent living and financial autonomy.
Neurological development in children born moderately or late preterm
Mitha, Ayoub, Ruoqing Chen, Neda Razaz, Stefan Johansson, Olof Stephansson, Maria Altman, and Jenny Bolk. “Neurological Development in Children Born Moderately or Late Preterm: National Cohort Study.” BMJ, January 24, 2024, e075630. https://doi.org/10.1136/bmj-2023-075630.
Children born moderately (32-33 weeks) or late (34-36 weeks) preterm face increased risks of neurodevelopmental impairments compared to term-born peers. However, most studies have focused on extremely (<28 weeks) or very (28-31 weeks) preterm infants, despite moderately and late preterm infants comprising nearly 80% of all preterm births. As these infants often receive the same routine care as term-born infants, understanding their long-term outcomes is helpful for healthcare planning and parental counselling.
This Swedish nationwide cohort study by Mitha et al. investigated the neurodevelopmental outcomes of 1,281,690 moderately preterm, late preterm, and term-born infants up to age 16 years.
The researchers found that moderately and late preterm infants had higher risks of motor, cognitive, visual, and hearing impairments compared to term-born infants, with risks highest at 32 weeks and gradually decreasing until 41 weeks. Early term (37-38 weeks) infants also showed increased risks.
These findings highlight the importance of considering the full spectrum of prematurity when planning delivery, assessing neurodevelopmental risks and planning follow-up care.
Peripartum extracorporeal cardiopulmonary resuscitation and rescue aspiration pulmonary embolectomy
An impressive case report here of a 43-year-old primigravida with worsening dyspnea followed by cardiac arrest due to massive pulmonary embolism (PE) shortly after emergency cesarean delivery. Extracorporeal cardiopulmonary resuscitation (ECPR) was initiated within 25 minutes. CT confirmed bilateral PE, and the patient underwent successful aspiration embolectomy using a Triever catheter system.
She was weaned off ECPR after 26 hours and discharged home with her child on day 7, achieving full recovery. The newborn had Apgar scores of 9 and 10. This case highlights the successful use of ECPR and percutaneous catheter-based interventions in managing peripartum PE when thrombolysis is contraindicated. The multidisciplinary approach and timely interventions led to a favourable outcome for both Mum and baby.
Finally, a few extras to finish…